If you're wondering, "does psoriatic arthritis really cause hair loss?"—you're not alone. Many living with PsA notice sudden hair thinning or scalp irritation and start to worry. This article explains the real connection between psoriatic arthritis and hair loss, the science behind it, and how you can manage or even reverse it. You’ll learn from …
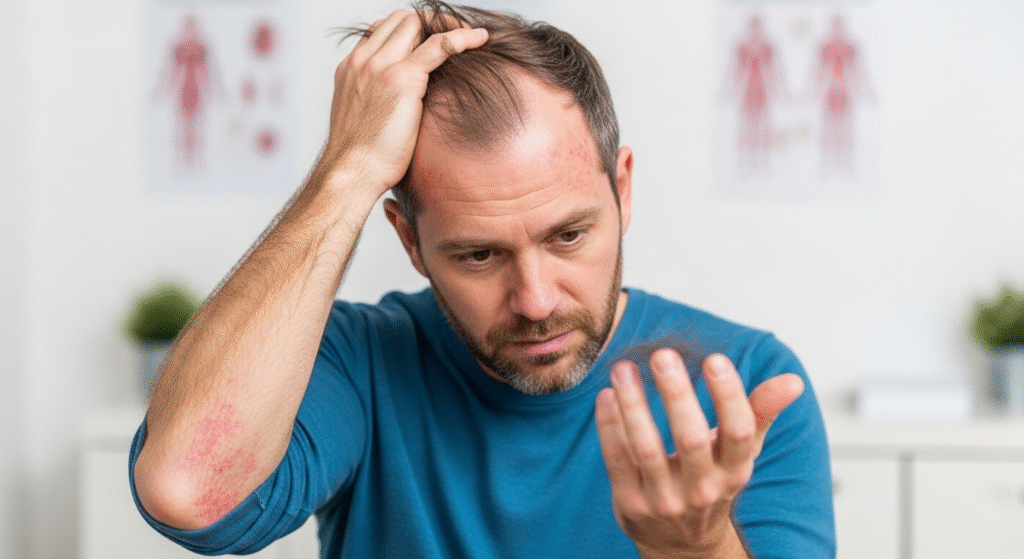
If you’re wondering, “does psoriatic arthritis really cause hair loss?”—you’re not alone. Many living with PsA notice sudden hair thinning or scalp irritation and start to worry.
This article explains the real connection between psoriatic arthritis and hair loss, the science behind it, and how you can manage or even reverse it. You’ll learn from expert insights, recovery timelines, and patient experiences to help you take back control—with confidence and clarity.

What Is Psoriatic Arthritis and How Is It Related to Hair Loss?
Understanding Does Psoriatic Arthritis Really Cause Hair Loss
Psoriatic arthritis (PsA) is a chronic autoimmune condition that causes inflammation in the joints and often affects individuals who already have psoriasis. It leads to joint pain, stiffness, swelling—and yes, in some cases, hair loss. The key culprit here is inflammation.
When inflammation affects the scalp, or when systemic flares increase stress on the body, hair follicles can shift prematurely into the telogen (resting) phase, leading to noticeable shedding.
How PsA Triggers Hair Loss
- Immune system attacks not just the joints but also skin and scalp.
- Scalp psoriasis causes flaking, plaques, and scratching, damaging hair follicles.
- Stress from chronic illness can trigger telogen effluvium (temporary hair shedding).
Types of Hair Loss Associated with PsA

Psoriatic Alopecia
This type of hair loss is directly tied to psoriasis on the scalp. Inflammation, itching, and the buildup of scales weaken follicles, sometimes causing bald patches. While usually temporary, repeated damage can slow regrowth.
Telogen Effluvium
This occurs when the body undergoes stress—like a PsA flare-up. Hair enters a resting phase and starts to shed about 2–3 months later. It’s diffuse (all over the scalp), not patchy.
Alopecia Areata (Rare)
In a few cases, autoimmune conditions like PsA may co-occur with alopecia areata, leading to patchy baldness. Though rare, it’s worth discussing with a dermatologist if bald spots appear suddenly.
Key Risk Factors and Medication Considerations
Scalp Psoriasis
Scalp involvement increases your risk. Constant scratching or picking at plaques can injure hair roots and delay regrowth.
Common symptoms include:
- Red, scaly patches
- Itching or burning sensations
- Silvery scales in hairline or crown
PsA Medications and Hair Loss
Some treatments for PsA may ironically contribute to hair shedding:
- Methotrexate: Can cause telogen effluvium in some patients.
- TNF-α inhibitors (like adalimumab): Rarely lead to alopecia areata-like symptoms.
- Biologics: Generally safe, but responses vary per patient.
Pro Tip: Never stop medication without medical supervision. Instead, talk to your rheumatologist about options.
Stress and Hormonal Factors
Chronic illness often elevates cortisol levels, which impact hair growth cycles. Managing stress is just as vital as treating inflammation.
Hair Regrowth Outlook and Recovery Timeline
Will Your Hair Grow Back?
Yes—in most cases, hair regrows once inflammation is under control or medications are adjusted. However, it may take weeks to several months.
Sample Recovery Timeline
| Phase | What’s Happening | Timeline |
|---|---|---|
| Flare or medication trigger | Hair roots enter resting phase | 0–2 weeks |
| Shedding phase begins | Noticeable hair fall | 2–3 months post-trigger |
| Recovery phase | Follicles restart growth | 4–6 months |
| Full regrowth | Normal thickness restored | 6–12 months |
When Hair Loss May Become Permanent
If scalp psoriasis leads to scarring alopecia or repeated trauma to follicles, regrowth may be limited. Early treatment is key.
Treatment Options and Scalp Care
Medical Treatments
- Topical corticosteroids: Reduce inflammation and scaling.
- Coal tar or salicylic acid shampoos: Help lift scale buildup.
- Biologic drugs: Control PsA systemically (e.g., apremilast, secukinumab).
- Vitamin D analogs: Promote follicle health.
Gentle Scalp Care Tips
- Avoid hot water; use lukewarm.
- Brush gently using a wide-tooth comb.
- Use sulfate-free, anti-inflammatory shampoos.
- Moisturize your scalp regularly.
Pro Tip: Trim nails and avoid scratching during flares to prevent follicle trauma.
Lifestyle and Diet for Hair and PsA Health

- Omega-3s (fish oil), biotin-rich foods, and leafy greens help reduce inflammation.
- Limit alcohol and sugar intake.
- Prioritize sleep, hydration, and stress reduction (yoga, therapy, meditation).
EEAT and Real‑World Perspectives
Case Study: Patient Recovery
One patient using apremilast for PsA reported:
- Significant hair regrowth within 3 months
- Reduced scaling and less itch after switching to coal tar shampoo
- Full recovery of volume by month 6
FAQ
Does PsA directly cause permanent hair loss?
Not usually. Most hair loss linked to PsA is temporary and regrows with treatment.
Can changing medications stop the hair loss?
Yes. Speak with your rheumatologist—some medications may be switched to better suit your body’s response.
How long does shedding last after a flare?
It can start 6–8 weeks after a trigger and continue for several months.
Can I treat scalp psoriasis and still dye my hair?
It’s best to avoid dyes during flares. Use scalp-friendly products and consult your dermatologist.
Should I see a dermatologist or rheumatologist?
Both! A rheumatologist treats PsA systemically, while a dermatologist addresses scalp symptoms.
Ready To Take Your Next Step
If you’re dealing with PsA and experiencing hair loss, don’t wait. Early diagnosis and the right care plan can make all the difference.
Book a consultation with Dr. Uzma Irfan, an ISHRS-certified surgeon in Islamabad today to uncover your best treatment path for hair regrowth and PsA management.